A nurse is performing a preoperative assessment on four clients, each with unique medical histories and reasons for surgery. This comprehensive assessment plays a crucial role in ensuring optimal patient outcomes and minimizing surgical risks. The assessment involves a thorough review of each client’s medical history, physical examination, and laboratory tests, providing valuable information to guide perioperative care.
This guide will delve into the essential components of a preoperative assessment, highlighting the importance of accurate and comprehensive documentation. It will also discuss nursing interventions based on assessment findings, emphasizing the significance of patient education and monitoring.
Client Information

The four clients undergoing preoperative assessments are:
- Client A: A 65-year-old male with a history of hypertension and diabetes mellitus, scheduled for a coronary artery bypass graft (CABG).
- Client B: A 42-year-old female with a history of breast cancer, scheduled for a mastectomy.
- Client C: A 25-year-old male with a history of trauma, scheduled for an exploratory laparotomy.
- Client D: A 38-year-old female with a history of obesity, scheduled for a laparoscopic gastric bypass.
Assessment Procedures: A Nurse Is Performing A Preoperative Assessment On Four Clients
A comprehensive preoperative assessment involves the following steps:
- Medical history review
- Physical examination
- Laboratory tests
- Assessment of the client’s understanding of the surgical procedure and postoperative care
The assessment tools used include:
- Health history questionnaire
- Physical examination form
- Laboratory test results
Physical Examination
The physical examination components relevant to preoperative assessment include:
- Vital signs: Blood pressure, heart rate, respiratory rate, and temperature
- Respiratory assessment: Auscultation of breath sounds, percussion of the chest, and assessment of respiratory effort
- Cardiovascular assessment: Auscultation of heart sounds, palpation of pulses, and assessment of peripheral edema
- Abdominal assessment: Auscultation of bowel sounds, palpation of the abdomen, and assessment of liver and spleen size
Medical History Review
Reviewing the client’s medical history is important to identify potential risks and complications.
Specific areas of inquiry include:
- Allergies
- Medications
- Previous surgeries
- Current health problems
- Family history of medical conditions
Laboratory Tests
Common laboratory tests performed as part of preoperative assessment include:
- Complete blood count (CBC)
- Electrolytes
- Coagulation studies
- Blood type and crossmatch
- Urinalysis
These tests provide information about the client’s overall health status, including their blood count, electrolyte balance, coagulation status, and kidney function.
Nursing Interventions
Based on the assessment findings, the nurse develops a plan of care that includes the following interventions:
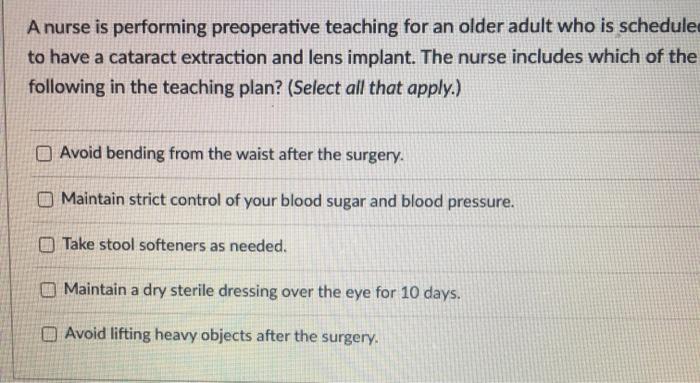
- Preoperative teaching: Educating the client about the surgical procedure, postoperative care, and potential risks and complications
- Medication administration: Administering medications as prescribed by the surgeon
- Patient monitoring: Monitoring the client’s vital signs, respiratory status, and level of consciousness
Documentation, A nurse is performing a preoperative assessment on four clients
Accurate and comprehensive documentation is essential for preoperative assessment.
The types of documentation used include:
- Nursing notes
- Progress reports
- Preoperative checklist
These documents provide a record of the client’s assessment findings, interventions, and progress.
Questions Often Asked
What is the purpose of a preoperative assessment?
A preoperative assessment aims to gather comprehensive information about a patient’s medical history, physical condition, and laboratory values to identify potential risks and optimize surgical outcomes.
What are the key components of a preoperative assessment?
A preoperative assessment typically includes a medical history review, physical examination, and laboratory tests, such as blood counts, electrolytes, and coagulation studies.
Why is documentation important in preoperative assessment?
Accurate and comprehensive documentation ensures clear communication among healthcare providers, facilitates continuity of care, and provides a legal record of the patient’s condition and the assessment findings.

