Nursing diagnosis of Cushing syndrome, a complex endocrine disorder, presents a unique challenge in patient care. This guide delves into the pathophysiology, clinical manifestations, risk factors, and diagnostic criteria of Cushing syndrome, empowering healthcare professionals with the knowledge and skills to effectively manage this condition.
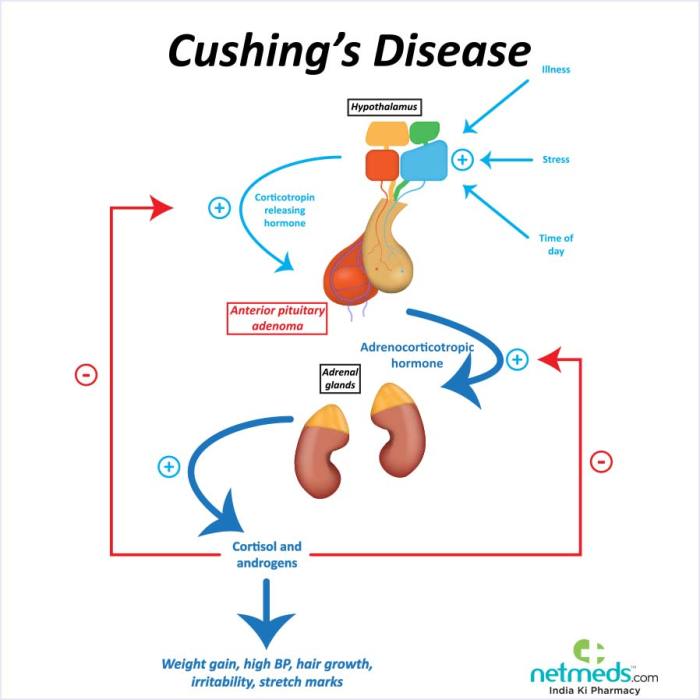
Understanding the intricate mechanisms underlying Cushing syndrome is crucial for developing targeted interventions. The hypothalamic-pituitary-adrenal (HPA) axis plays a central role in the development of this disorder, and its dysregulation leads to the characteristic clinical manifestations observed in patients.
Pathophysiology
Cushing syndrome arises from excessive exposure of tissues to glucocorticoids, resulting in a complex pathophysiology. The primary underlying mechanism involves a dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, leading to increased production of cortisol.
In normal physiology, the HPA axis functions as a feedback loop:
- The hypothalamus releases corticotropin-releasing hormone (CRH).
- CRH stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH).
- ACTH triggers the adrenal glands to produce cortisol.
- Elevated cortisol levels provide negative feedback to the hypothalamus and pituitary gland, suppressing further CRH and ACTH release.
In Cushing syndrome, this feedback loop is disrupted, resulting in excessive cortisol production. This can occur due to:
- Pituitary adenomas (ACTH-dependent Cushing syndrome)
- Ectopic ACTH production (ACTH-independent Cushing syndrome)
- Primary adrenal gland tumors (primary Cushing syndrome)
- Iatrogenic administration of glucocorticoids
Clinical Manifestations
Cushing syndrome presents with a wide range of clinical manifestations that can be categorized as follows:
Physical, Nursing diagnosis of cushing syndrome
- Central obesity (predominantly in the face, neck, and abdomen)
- Thinning skin
- Easy bruising
- Purple striae
- Hirsutism
- Acne
- Osteoporosis
- Muscle weakness
Metabolic
- Hyperglycemia
- Insulin resistance
- Dyslipidemia
- Hypertension
Psychological
- Mood swings
- Depression
- Anxiety
- Cognitive impairment
Risk Factors and Causes
Cushing syndrome can develop in individuals of any age or gender. However, certain factors increase the risk, including:
- Prolonged use of glucocorticoids
- Pituitary adenomas
- Ectopic ACTH production (e.g., from lung or bronchial carcinoid tumors)
- Primary adrenal gland tumors (e.g., adrenocortical carcinoma)
- Multiple endocrine neoplasia type 1 (MEN1)
- Familial Cushing syndrome
The following table compares the different types of Cushing syndrome based on their etiology:
| Type | Etiology |
|---|---|
| ACTH-dependent Cushing syndrome | Pituitary adenomas (Cushing disease) |
| ACTH-independent Cushing syndrome | Ectopic ACTH production |
| Primary Cushing syndrome | Adrenal gland tumors (e.g., adrenocortical carcinoma) |
| Iatrogenic Cushing syndrome | Exogenous glucocorticoid administration |
Diagnostic Criteria
The diagnosis of Cushing syndrome requires a comprehensive evaluation, including:
Laboratory Tests
- 24-hour urine free cortisol
- Late-night salivary cortisol
- Dexamethasone suppression test
- ACTH level
Imaging Studies
- Magnetic resonance imaging (MRI) of the pituitary gland
- Computed tomography (CT) scan of the adrenal glands
- Octreotide scan (for ectopic ACTH production)
Differential Diagnosis: Nursing Diagnosis Of Cushing Syndrome
The differential diagnosis of Cushing syndrome includes conditions that can mimic its clinical manifestations, such as:
- Obesity
- Polycystic ovary syndrome (PCOS)
- Acromegaly
- Depression
- Hypothyroidism
The following table Artikels the key differentiating features between Cushing syndrome and its mimics:
| Feature | Cushing Syndrome | Obesity | PCOS | Acromegaly | Depression | Hypothyroidism |
|---|---|---|---|---|---|---|
| Central obesity | Yes | Yes | Yes | No | No | No |
| Thinning skin | Yes | No | No | No | No | No |
| Easy bruising | Yes | No | No | No | No | No |
| Purple striae | Yes | No | No | No | No | No |
| Hirsutism | Yes | Yes | Yes | No | No | No |
| Hyperglycemia | Yes | No | No | No | No | No |
| Mood swings | Yes | Yes | Yes | No | Yes | Yes |
FAQ Corner
What are the common signs and symptoms of Cushing syndrome?
Cushing syndrome presents with a range of signs and symptoms, including weight gain, central obesity, facial rounding, skin thinning, easy bruising, muscle weakness, fatigue, and impaired glucose tolerance.
How is Cushing syndrome diagnosed?
Diagnosis of Cushing syndrome involves a combination of clinical evaluation, laboratory tests, and imaging studies. Blood and urine tests can measure cortisol levels, while imaging studies, such as MRI or CT scans, can visualize adrenal tumors or pituitary lesions.
What are the treatment options for Cushing syndrome?
Treatment for Cushing syndrome depends on the underlying cause and may include medications, surgery, or radiation therapy. Medications can block cortisol production or reduce its effects, while surgery aims to remove adrenal tumors or pituitary lesions.